 Not all patients have the same genetic make up - it is estimated that differences between individuals account for 20-95% of variability in drug dispositions and effects. This means that the benefits of a single drug may only be evident in a subset of patients, rather than being uniform across the whole population.
Not all patients have the same genetic make up - it is estimated that differences between individuals account for 20-95% of variability in drug dispositions and effects. This means that the benefits of a single drug may only be evident in a subset of patients, rather than being uniform across the whole population.
Pharmacogenomics is a field of science that uses information about an individual’s genes, proteins and environment to predict an individual’s response to certain drugs, and create a personalized treatment.
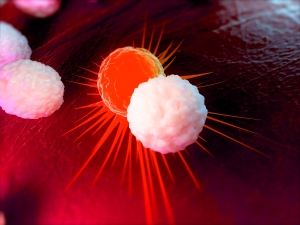
Finding unique patterns in an individual’s genetic makeup through “biomarker” analysis, allows the identification of groups of patients who have the same molecular variation of the disease, and thus, may benefit from a certain drug or combinations of drugs. Identification of the right group of drugs for a patient leads to 1) a higher probability of successful treatment, 2) reduces the probability of negative side effects. For example, in breast cancer, there are a number of gene expression signatures that have been developed that can be used to estimate prognosis for an individual patient based on assessment of the tumour. In patients who have a form known as “HER-2+ breast cancer”, overexpression of the HER-2 gene leads to a higher than normal expression of the HER-2 receptor in breast cancer cells. The drug, trastuzumab, was been developed specifically to interfere with the receptor. A number of next-generation drug combinations have recently become available, allowing treatments to be further personalised with a greater chance of successful treatment. More recently, pharmacogenomics has been applied to an exciting new field known as immuno-oncology (I/O). These treatments use an individual’s own immune system to help fight cancer through use of a single I/O drug or combinations of drugs. Normally, white blood cells known as “T-cells” in an individual’s immune system recognize cancer cells as foreign and attack and kill the problem cells. Certain types of cancer exhibit molecules on their surface, known as PD-L1. Interaction with the T-cell surface molecule (known as PD-1) protects the cancer cell from being attacked by T-cells. However, this attack can be reactivated by drugs that block the PD-L1/ PD-1 interaction. To date, single agent anti-PD-1 / PD-L1 has demonstrated survival benefit in five cancer types - bringing hope to many patients who previously had very few treatment options. The next wave of innovation is to develop effective I/O combination treatments to address patients who do not benefit from monotherapies, and in this regard, it is critical to co-develop a biomarker that will guide treatment selection. AstraZeneca, Bristol-Myers Squibb, Merck and Roche are key players in the Pharmaceutical industry who are leading I/O combination therapy development. The scientific and medical communities are excited to see data in the coming years, with new presentations at the cancer conference, American Society Of Clinical Oncology, in June 2017.
As the options for personalized medicines expand, biomarkers will also play an important role beyond the lab and the clinic.
They will be vital in ensuring patients receive the most effective combination of treatments at a time when healthcare budgets are under significant pressure.
Eleanor Fung
Director - Global Product & Portfolio Strategy at AstraZeneca
Further reading: Molecular Oncology 2012, 6: 140 Semin Oncol. 2016 43:501. J Immunother Cancer. 2016; 4:48 Lancet Oncol. 2016;17:e347-62 www.cancer.gov